What should I know about back pain?
Back pain is a very common problem and will affect many of us at some point during our lives.
The good news is that in most cases it isn’t a serious problem, and it might just be caused by a simple strain to a muscle or ligament.
As far as possible, it’s best to continue with your normal everyday activities as soon as you can and to keep moving.
Being active and exercising won’t make your back pain worse, even if you have a bit of pain and discomfort at first. Staying active will help you get better. Taking painkillers can help you do this.
How your back works
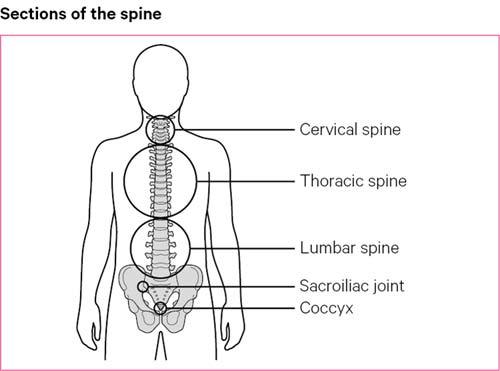
The spine, which is also called the backbone or spinal column, is one of the strongest parts of the body and gives us a great deal of flexibility and strength.
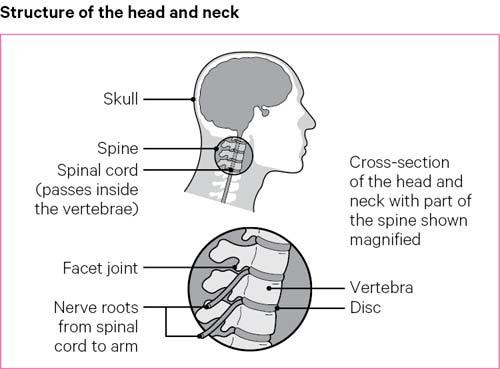
It’s made up of 24 bones, known as vertebrae, one sitting on top of the other. These bones have discs in between and lots of strong ligaments and muscles around them for support. There are also the bones in the tailbone at the bottom of the back, which are fused together and have no discs in between.
On either side of the spine, running from top to bottom, are many small joints called the facet joints.
The spinal cord passes inside the vertebrae, which protect it.
The spinal cord connects to the brain through the base of the skull and to the rest of the body by nerves that pass through spaces between the bones of the spine. These nerves are also known as nerve roots.
As you grow older, the structures of your spine, such as the joints, discs and ligaments, age as well. The structures remain strong but it’s usual for your back to get stiffer as you get older.
Causes
Often back pain doesn’t have one simple cause but may be due to one or more of the following:
- poor posture
- lack of exercise resulting in stiffening of the spine and weak muscles
- muscle strains or sprains.
As well as the things listed above, there are also specific conditions which are linked with pain felt in the back. It’s important to remember that severe pain doesn’t necessarily mean there’s a serious problem. Some common conditions are listed below.
Spondylosis
As we grow older, the bones, discs and ligaments in the spine can naturally weaken as they age. This happens to all of us to some degree as part of the ageing process, but it doesn’t have to be a problem and not everyone will have pain from this.
As we grow older the discs in the spine become thinner and the spaces between the vertebrae become narrower. Little pieces of bone, known as osteophytes, may form at the edges of the vertebrae and facet joints.
The medical term for this is spondylosis and is very similar to the changes caused by osteoarthritis in other joints.
Keeping the spine supple and the muscles around the spine and pelvis strong, will reduce the impact of spondylosis.
Sciatica
Back pain is sometimes linked with pain in the legs, and there may be numbness or a tingling feeling. This is called sciatica.
This is due to a nerve in the spine being pressed on or squeezed. For most people with sciatica, the leg pain can be the worst part and occasionally they may have little or no back pain at all.
In most cases sciatica is caused by a bulging disc pressing on the nerve. Discs are designed to bulge so we can move our spines about easily, but sometimes a bulge can ‘catch’ a nerve root and cause pain that travels all the way down the leg and foot.
Most people recover fairly quickly, although in some cases it might take a number of months.
Starting gentle exercise as soon as you can will greatly help with sciatica. It is also a very good idea to see a physiotherapist.
Spinal stenosis
Sometimes back pain is linked with pain in the legs which starts after you start walking for a few minutes, and then tends to get better very quickly when you sit down. This is known as spinal stenosis.
This can happen from birth or can develop as we get older.
Problems are caused when something presses on the small space in the middle of the spine, where the nerves are. This space, which is called the spinal canal or nerve root canal, can be squeezed by bone or ligament.
Symptoms often affect both legs, but one may be worse than the other. The pain usually gets better when you sit down and rest, and some people find they have less pain if they walk a little stooped. Like sciatica, the main problem tends to be leg pain more than the back pain.
In most cases, neither sciatica nor spinal stenosis are serious problems. However, if the symptoms cause you a lot of trouble and greatly affect your quality of life then you should see your doctor for further advice and to discuss what else can be done.
Other causes
Other rarer causes of back pain include:
- bone problems such as a fracture – often linked to thinning of the bones, which is known as osteoporosis
- an infection
- a tumour
- inflammation, for example in the condition ankylosing spondylitis.
When to see a doctor
Even though it's common, most cases of back pain tend to clear up without the need to see a doctor.
You should see your doctor if your pain:
- is really bad
- lasts for a long time
- stops you from working or doing the things you enjoy
- affects your everyday activities
- gets worse.
You should also see your doctor if you have any changes in sexual function, for example, being unable to get an erection.
If the pain is causing you significant problems and stops you from getting on with normal life and work activities, your doctor will examine you and ask you questions.
These questions will help predict how likely it is that you need further help with your back pain. If you do need further support, your doctor will make a referral to physiotherapy so that you can have treatment early, to help with the pain and return to normal activities.
It’s natural to want to know what has caused your back pain. However, specialists may not be able to tell you for certain what has caused your back pain, even after carefully assessing you.
If you’re concerned about the cause of your back pain, it can help to talk openly about any worries with a healthcare professional, as reducing any fear may help speed up your recovery.
What are the warning signs of a serious problem?
Very rarely back pain or pain that travels down the leg is a sign of a serious problem.
If you have any of the following symptoms, you should seek urgent medical attention:
- difficulty controlling or passing urine
- loss of control of your bowels
- numbness around your back passage or your genitals
- serious weakness in your legs so you find standing really difficult
- severe and ongoing back pain that gets worse over several weeks.
The above symptoms could potentially be linked to a rare but serious condition that needs urgent medical attention.
Diagnosis
National guidelines suggest that doctors should use a common-sense ‘wait and see’ approach when diagnosing back pain before deciding if you need further treatment, especially as most cases of back pain improve by themselves. As a patient this approach can sometimes be frustrating, but you may find that if you keep up your self-help measures, you won’t need further treatment anyway.
Should you need further treatment, your GP will be able to assess your back pain by discussing your symptoms with you. Most problems can be diagnosed after a simple examination, and it’s unlikely that any special tests will be needed.
Tests
You may be sent for tests if:
- you’ve had an injury to your back, for example a bad fall
- your doctor suspects that there may be an underlying cause for your pain
- the pain has lasted for an unusually long time.
In this case a magnetic resonance imaging (MRI) scan or computerised tomography (CT) scan may be needed.
X-rays are much less commonly used because back pain is often caused by problems with soft tissues, such as ligaments and muscles, which can’t be seen on x-rays.
Changes to the spine as a result of spondylosis can show up on x-rays. These common changes that happen to us all can appear on x-rays without people having any pain or problems. Because of this, x-rays aren’t particularly helpful.
Remember that sometimes even after a thorough investigation it might not be possible to say for certain what is causing back pain.
Managing your symptoms
The most important things to do to treat back pain is to keep moving, continue with everyday activities and have a healthy lifestyle.
Some people worry that if they have back pain, doing certain activities such as lifting things, twisting and turning might make their back pain worse. It’s important to remember that our backs and our spines are very strong and are designed to move.
In fact, too much rest can make back pain worse.
Being active and continuing with your everyday activities as soon as possible, and as much as possible, will speed up your recovery.
There’s also evidence to suggest that how you respond emotionally to having back pain has an important impact on how quickly you get better. The more positive you are, the more active you are, the quicker your back will get better.
Remember, if you’re ever struggling don’t suffer in silence, talk to a healthcare professional.
Keep moving
Staying active is the most important way you can help yourself if you have back pain.
Keeping the muscles around the spine strong, will provide more support to the bones and joints and take pressure off them. The more you move, the more the back will keep its natural range of movement.
If you stop being active for a long time, the muscles in your back become weak and you become less fit, and this can make your back pain worse. Not moving can make your back more stiff and painful.
Regular exercise leads to shorter and less frequent episodes of back pain. It also releases chemicals called endorphins, which are the body’s natural painkillers. These improve pain and make you feel happier.
Exercise might make your back feel a bit sore at first but it doesn’t cause any harm – so don’t let it put you off. If you're getting back to exercise, start off gently and gradually increase the amount of exercise you do. Regular and small episodes of exercise is a good way to start and then each day try to do a little bit more.
Try taking some painkillers beforehand too. Over time, your back will get stronger and more flexible, and this should reduce pain.
Types of exercise for back pain
It’s better to choose a form of exercise that you enjoy as you’re more likely to stick to it. There are many forms of exercise that have helped people with back pain. Examples include:
- swimming
- walking
- yoga
- Pilates
- going to the gym.
Research has found that a specially developed 12-week yoga programme can help people with low back pain lead more active lives and manage their condition more effectively. Many of the people who took part in the study also found that they had the knowledge to prevent further attacks if they felt an episode of back pain coming on.
You can find more information about the 12-week programme at www.yogaforbacks.co.uk
Many community and sports centres also run yoga classes if you’re interested in trying it. Make sure you speak to the yoga instructor before you start so they’re aware that you have back pain.
You can find some examples of exercises you might like to try to reduce your pain on our exercises for the back page.
Pain during exercise
You may feel some discomfort and sometimes pain when you exercise. This feeling is normal and should calm down a few minutes after you finish. It’s not a sign that you're hurting yourself. Exercise will help reduce pain and can help you manage your back pain better.
While you can push yourself and do strenuous exercise, it’s important not to overdo it. If you are in pain that you can’t cope with during or after your activity, you will need to see a doctor. The key is to start off gently and to gradually increase the amount you do.
Often people stop exercising once their back pain has cleared up. But if you stop exercising all the improvements you’ve made will disappear within a few weeks. So, it’s important that you continue to exercise regularly and don’t stop when the pain is gone and you’re feeling better.
If you’re ever having any trouble exercising, it can be a good idea to see a GP or ask for a referral to a physiotherapist for tailored exercise advice. If you're a member of a gym, there may well be personal trainers there who can give you expert advice. Make sure you tell them about your condition.
Painkillers
Simple painkillers such as paracetamol may help to reduce symptoms and allow you to continue with your everyday activities. You should use them as and when you need them but it’s best to take them before the pain becomes very bad. It’s important that you take them regularly and at the recommended dose, especially when you’re having a flare-up of your back pain.
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, which you can buy at chemists and supermarkets, can also help.
You can use painkillers and NSAIDs for a short course of treatment of about a week to 10 days. If they’ve not helped after this time, then they’re unlikely to. However, if they do help but the pain returns when you stop taking them, you could try another short course.
There are also anti-inflammatory creams or gels that can be rubbed onto affected areas. Be careful not to exceed the dose by taking an NSAID tablet and applying an NSAID cream at the same time.
If you have any questions or concerns about what drugs you can take and the dosage, talk to a doctor or a pharmacist.
Sometimes other drugs are used to treat back pain if you’re really struggling with the pain. Read our treatments section for more information.
Heat/ice packs
Applying a heat pack to the affected area can ease pain and stiffness. You can use a reusable heat pad which you can buy from chemists and sports shops, a microwavable wheat bag or a hot-water bottle.
A warm bath or hot shower can have a similar soothing effect.
An ice pack bought from a chemist, or even just a bag of frozen peas, can also be helpful.
You may find that alternating between heat and ice therapy throughout a day or week can help.
You could experiment with hot and cold packs to find what works best for you.
Make sure you protect your skin from direct contact with heat or ice packs to avoid burns or irritation of your skin. A tea towel over the heat or ice pack is one way to do that. Read the instructions carefully if you have bought a heat or ice therapy product. Applying ice or heat for about 15 to 20 minutes at a time is normally enough.
Posture
Try to maintain good posture when sitting at home, at work or in the car. Staying in awkward positions while working or driving, for example, will affect the soft tissues in your back that support your spine, and will increase your pain or your recovery time.
Try to change your posture often, because remaining in the same position for too long can be bad for you.
Complementary medicine
There are many different complementary treatments that are believed to help with pain relief, and some people do feel better when they use them.
However, on the whole these treatments aren’t recommended for use on the NHS because there’s no proof that they definitely work.
Acupuncture
Sometimes acupuncture might provide pain relief. It’s thought to work by diverting or changing the painful sensations that are sent to the brain from painful tissues and by stimulating the body’s own pain-relieving hormones, known as endorphins.
Massage
Massage is a manual technique which uses rhythmic strokes, kneading or tapping actions to move the muscles and soft tissue of the body. Massage can reduce anxiety and stress levels, ease muscular tension and fatigue, and improve circulation, which all work to reduce pain levels.
Lifting correctly
Learning to lift correctly may help to prevent further episodes of back pain.
Bend your knees when lifting and allow your spine to move as necessary, without twisting it. When doing tasks like carrying shopping, try and split the load between both hands. Keeping the weight close to your body also helps.
Diet and nutrition
There are no special diets that have been shown to either help or prevent back pain.
However, if you’re overweight you should consider changing your diet and doing some regular exercise to help you lose weight, as this will reduce the strain on your back.
What’s recommend for us all is a well-balanced and healthy diet, which is low in saturated fats, sugar and salt. It’s also a very good idea to eat plenty of fresh fruit and vegetables, and to drink plenty of water.
If you need to lose weight, the key is to regularly burn off more energy than you consume on a daily basis.
Read more about diet.
Pain management programmes
Pain management programmes may help you control your pain and teach you how to live with long-term pain. They’re usually outpatient sessions and involve learning about pain from a physical point of view, but also how it affects your mood and emotional well-being. The sessions will then look at what you can do to overcome difficulties.
Read more about pain and arthritis.
Related information
-
Let's Move with Leon
Sign up to Let’s Move with Leon our weekly email programme of 30-minute movement sessions, presented by fitness expert Leon Wormley.
-
Let's Move
Sign up to Let’s Move to receive a wide range of content about moving with arthritis – from exercise videos to stories and interviews with experts – straight to your email inbox.
Treatment
Taking some painkillers, staying active and doing some specific exercises are generally the most helpful treatments for people with back pain. However, some people will need further medical treatment.
Therapies
Physiotherapy
Physiotherapy can be useful to improve your strength and flexibility. Exercise is one of the most effective treatments for back pain. A physiotherapist can help oversee your exercise programme and recommend specific exercises to help.
Manual therapies, which are sometimes called ‘hands-on’ treatments, such as manipulation and mobilisation of the spinal joints, can help to clear up a spell of back pain along with exercises. These manual therapy techniques are usually carried out by osteopaths, chiropractors and physiotherapists.
These therapies might not be suitable for all back conditions. Talk to your doctor if you’re thinking of trying one of these. And make sure you explain to the therapist what condition you have.
Read more about physiotherapy.
Occupational therapy
If your back pain is causing problems with daily activities such as dressing, washing and driving, you may find it useful to see an occupational therapist. They may suggest different ways of doing things to reduce the strain or recommend aids or gadgets that will help you. However, it’s important that you don’t come to rely on aids or gadgets instead of trying to get back to your daily activities.
Find out more about occupational therapy.
Talking therapies
Back pain, especially if it lasts for a long time, can affect people’s mood. If you are feeling really low or anxious, it’s important to talk to someone such as a partner, relative, friend or a doctor. ‘Talking therapies’ can be useful.
For example, cognitive behaviour therapy (CBT) can help people with back pain. The aim is to help people to deal with problems in a more positive way, by breaking them down into smaller parts. Your doctor may be able to refer you for CBT, or you might like to consider going private.
Keeping socially and physically active is an important part of helping with low mood and anxiety, and it also helps with pain. Simple things, such as joining a local leisure centre, sports club, walking group, gardening group, or just getting out and seeing friends for a coffee on a regular basis might really help you.
Drugs
If standard painkillers or NSAIDs aren’t working for you, your doctor may suggest some additional treatments.
Amitriptyline
Amitriptyline acts to relax muscles and improve sleep. You’ll usually be prescribed the lowest possible dose to control your symptoms. If the starting dose isn’t working, your dose can be gradually increased. This approach will help to lower the risk of side-effects, which can include a dry mouth, drowsiness and blurred vision.
If you experience these side-effects you should stop the medication and discuss this with your doctor.
Read more about amitriptyline.
Gabapentin/pregabalin
Gabapentin and pregabalin aren’t usually given as a first-line treatment for ‘ordinary’ back pain. Although they might not help much with back pain, they may help sciatica by reducing irritation of the nerves. They may need to be taken for six weeks to begin with, and sometimes longer.
As with all drugs there can be side-effects, so they won’t be suitable for everyone. You should discuss this with your doctor.
Injections
Sometimes injections are useful for back pain or sciatica which is more severe or if the usual treatments like physiotherapy and painkillers aren’t working well enough. For sciatica, these injections are called epidurals, and involve an injection of a steroid, which is a strong anti-inflammatory medicine, and anaesthetic, near the spine or through the tailbone, to try and help with pain from a ‘trapped’ nerve root.
Another type of injection, called radiofrequency denervation, might be used if it is thought that the back pain comes from natural changes that happen over time to the small joints in the spine called facet joints.
Your doctor will send you to see a specialist, to discuss if injections might be an option for your back pain or your sciatica pain. These injections are not always successful, but they do help some people.
Surgery
Very few people with back pain need an operation. Sometimes an operation is needed for spinal stenosis or for severe sciatica to free the nerve, although most doctors would recommend trying other measures first, including medication, physiotherapy or injections.
Urgent surgery may be needed if you lose bladder or bowel control or the use of your legs, but this is extremely rare.
Working with back pain
Getting back to work sooner rather than later will help most people with back pain.
This will help your back pain itself, as staying active and keeping the back muscles moving will help you get better sooner. It'll also make you feel better about yourself as time off work has been shown to affect people’s mood.
In the past, people were advised to rest up in bed and we now realise that it does more harm than good and that it's better to keep moving, even if you need to take some simple painkillers to allow you to do so.
Most people are able to return within 2-3 days, although the length of time off work varies with the individual and the type of job you do.
You don’t need to wait until your back problem has completely gone. In many cases, the longer you’re off work the more likely you are to develop longer-term problems and the less likely you are to return to work.
Getting support from your employer
It’s important to keep in contact with your employer and discuss what can be done to help you return to work. If your work involves heavy lifting or other physically demanding tasks, you may need to do lighter duties and fewer hours for a while.
If you have an occupational health advisor through your job, they can help advise what work you are fit to do and arrange any simple adjustments to your work or workplace to help you to cope and stay at work.
Getting other support
If you're having difficulties travelling to or from work or need an item of equipment, the Government’s Access To Work scheme might be able to help.
If you're unable to get back to work after two weeks of absence because of your back pain, you should talk to your GP and employer about getting physiotherapy or other treatment to get you moving again.
You can get further advice through your local Jobcentre Plus and the Government’s Fit for Work guidance.
Research and new developments
Our research has helped to improve the management of lower back pain. Researchers at our primary care centre in Keele developed the STarT Back Tool, which is used to help clinicians when deciding what treatment is needed for patients with lower back pain.
This targeted approach to treatment has been shown to lead to a reduction in patient-reported disability, fewer days off work and significant cost savings to both the NHS and the wider society. Use of the STarT Back Tool for non-specific low back pain is recommended by organisations including the Royal College of General Practitioners and NICE, and has been adopted by services both in the UK and worldwide.
We’re supporting research examining why some people with spondylosis in their lower spine have a lot of pain whilst others have little or no pain. This study will examine how people with and without low back pain move and function, and the results will help physiotherapists to deliver the right care to patients in the right way, making physiotherapy more effective and leading to improved outcomes and quality of life for patients.
We’re also looking at the role genes play in causing back pain. Our researchers are looking closely at bony lumps caused in spondylosis known as osteophytes, and the problems they can cause by putting pressure on nerves. For this work we’re using zebrafish to study spinal conditions with the aim to help understand how specific genes cause spinal osteoarthritis. Zebrafish are good models to use because of surprising similarities within their anatomy to the human spine.